The field of bioprinting is revolutionizing the way we understand human health and disease. Bioprinting, a subset of 3D printing, involves the creation of biomaterials such as cells, tissue, and even whole organs, through a process known as bioink printing. These bioprinted structures are used in a range of applications, from tissue engineering to drug testing, to the creation of prosthetics. But one of the most impactful uses of this technology continues to be in drug toxicity testing. Let’s dive deeper into the world of 3D bioprinting and explore how it’s changing the game in drug development.
Bioprinting: A Quick Overview
Bioprinting is a highly specialized field that combines the principles of biology, material science, and engineering. It begins with the extraction of live cells from a donor, be it human or animal. These cells are then used to create bioink, a substance used in the printing process.
Many different types of cells can be used to create bioink, including endothelial cells, which form the lining of blood vessels, and hepatocytes, the main cell type in the liver. The use of these cells allows for the production of highly accurate, organ-like structures, which can then be used in a variety of ways.
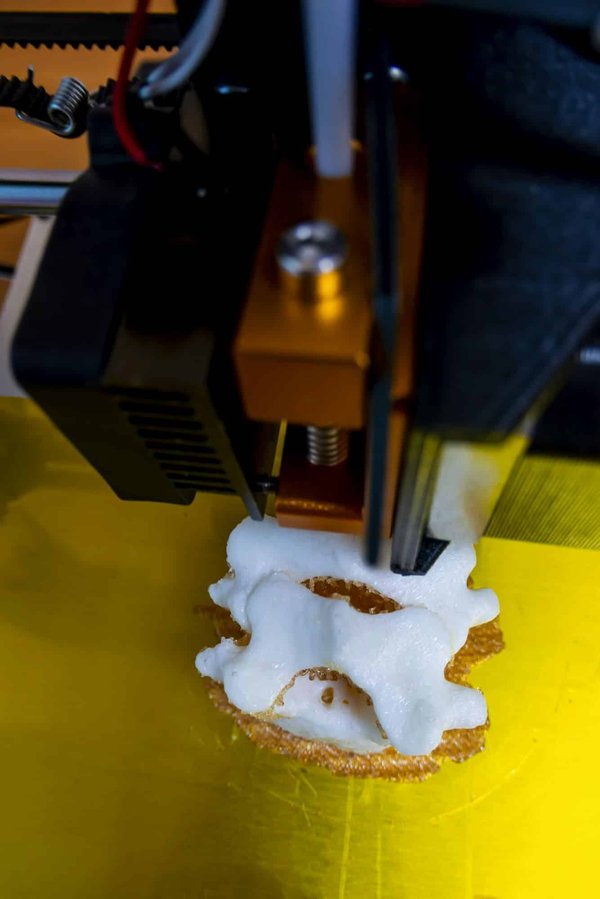
The bioprinting process itself is based on 3D printing technology. Like a traditional 3D printer, a bioprinter builds up layers of material – in this case, bioink – to create a 3D structure. But instead of plastic or metal, the "ink" in a bioprinter is a special type of gel that contains living cells.
The Role of Bioprinted Liver Tissues in Drug Toxicity Testing
In the realm of drug development, the liver plays a critical role. As the body’s primary detoxifying organ, the liver processes and breaks down drugs. It’s where potential toxins can be metabolized and excreted from the body. Consequently, drugs can have a high impact on the liver, leading to potential toxicity.
Traditionally, drug toxicity testing has been carried out on animals or in vitro cell cultures. However, these models are often inadequate, failing to accurately represent human physiology and response to drugs. This is where bioprinted tissues come in.
Bioprinted liver tissues offer a better representation of the human liver’s structure and function, providing more accurate results when it comes to testing drug toxicity. Bioprinted liver models incorporate both hepatocytes and endothelial cells, thus embodying the complex interactions within a real liver.
Benefits of Using Bioprinted Tissues in Drug Development
The use of bioprinted tissues in drug development offers a plethora of advantages. First and foremost, by using human cells to create the tissue models, researchers can gain a more accurate understanding of how a drug will react in the body.
This high degree of accuracy can potentially reduce the need for animal testing, a practice often fraught with ethical considerations. Furthermore, it can speed up the drug development process. With a more accurate model, fewer trial-and-error stages may be needed, resulting in faster progress from initial testing to clinical trials.
Bioprinted tissues also allow for personalized medicine. Cells can be taken from a particular individual and used to create a model of their liver. This liver can then be used to test how the individual would respond to different drugs, potentially allowing for highly personalized treatment plans.
Scholarly Insights into Bioprinting for Drug Toxicity Testing
The value and potential of bioprinting for drug toxicity testing are gaining recognition in the academic world. Scholars are increasingly investigating the benefits of bioprinted liver tissues and are acknowledging the significant role that bioprinting can play in the future of drug development.
In a study published in the Journal of 3D Printing in Medicine, researchers highlighted the potential of bioprinted liver tissues in predicting drug-induced liver injury. The study emphasized the advantages of using bioprinted liver models over traditional 2D cell cultures, citing the former’s superior ability to mimic human liver physiology.
Another research paper in the Journal of Applied BioMaterials & Bioengineering underscored the promise of 3D bioprinted liver models for personalizing drug testing. The researchers outlined a case where cells were taken from a patient with a rare liver disease, used to create a bioprinted liver model, and then used to test various treatment options.
That said, while the potential of bioprinting for drug toxicity testing is immense, it is still a developing field. There’s much more to learn and discover. What’s clear, however, is that this innovative technology is poised to play a significant role in the future of drug development, improving accuracy, reducing the need for animal testing, and paving the way for personalized medicine.
3D Bioprinting Techniques: Extrusion-Based Printing and Beyond
Fundamentally, bioprinting relies on a variety of techniques to print cell-laden bioink layers and create functional tissue models. One of the most common methods is extrusion-based printing, which deploys a continuous stream of bioink from a nozzle under pneumatic or mechanical pressure.
The extrusion-based method is well-suited for printing a broad array of cell types, including endothelial cells and hepatocytes. However, it’s important to note that this technique is not the only game in town. Other methods such as inkjet bioprinting, laser-assisted bioprinting, and stereolithography also have their merits.
Inkjet bioprinting, for instance, allows for high-speed printing, making it ideal for large-scale tissue engineering projects. Laser-assisted bioprinting, on the other hand, provides high resolution and precise cell placement, which is crucial for creating complex tissue structures. Lastly, stereolithography combines high precision with speed and versatility.
Such a range of techniques allows for the creation of 3D tissue models that closely mimic the intricate architecture of native tissues, thereby enhancing their potential for drug screening and personalized medicine.
The Future of Drug Discovery: Three Dimensional Bioprinting and Organ-on-a-Chip Technologies
Following the rise of bioprinting, another innovative technology is gaining traction in the field of drug development – organ-on-a-chip. This technology involves creating miniature versions of human organs on a microchip, enabling scientists to study the effects of drugs on organ function in real-time.
So, where does 3D bioprinting fit into this picture? Well, 3D bioprinting and organ-on-a-chip technologies can work in tandem to create even more accurate and representative models of human tissues and organs. 3D bioprinting provides the means to create the cell-laden tissue structures, while organ-on-a-chip technology allows for the dynamic and real-time analysis of these tissues under physiological conditions.
By integrating 3D bioprinting with organ-on-a-chip technologies, scientists could potentially create a "body-on-a-chip" – a system that mimics the entire human body’s response to drugs. This not only opens up new possibilities for drug screening but also takes us one step closer to the age of personalized medicine.
Conclusion: The Promise and Challenges of Bioprinting for Drug Toxicity Testing
While the potential of 3D bioprinting for drug toxicity testing is undeniably immense, the technology is still in its infancy. Many challenges need to be addressed, from improving the resolution of bioprinted tissues to ensuring their long-term stability and functionality.
Nevertheless, the advancements in this field so far have been promising. Scholarly insights from Google Scholar and various academic journals suggest that bioprinted liver tissues could be a game-changer in predicting drug-induced liver injury. In addition, the integration of bioprinting with other technologies like organ-on-a-chip could revolutionize the entire process of drug development.
In a world where diseases are becoming more complex and the demand for effective treatments is ever-increasing, bioprinting offers a ray of hope. By creating more accurate tissue models, reducing the reliance on animal testing, and paving the way for personalized medicine, 3D bioprinting might just be the breakthrough we need to herald a new era in drug discovery.
 1900Tr
1900Tr